Why Waiting Until Age 50 To Address Risk Factors For Heart Disease Is Too Late.

Most people only start to worry about cardiovascular risk later in life.
This is a bad idea.
Here’s why.
When you look at the risk of having a heart attack, it is true that the older you are, the greater the odds of having a heart attack1.

So far, so good.
But this graph is very misleading.
While only 1-2% of those having a heart attack are less than 65 years of age, 1-2% of this very large number means a LOT of heart attacks.
When you adjust for this fact and that there are a much smaller number of people alive over 85 years of age, you get a very different picture.
When viewed in this way, you can see that over half of all heart attacks in males and about 30% of all heart attacks in females happen at younger than 65 years of age.
Not good.

So why is it that so many people are having heart attacks at less than 65 years of age?
The reason:
They were accumulating plaque in their coronary arteries much earlier than their peers.
Remember.
You can’t have a heart attack if you don’t have plaque in your coronary arteries.
And plaque in your coronary arteries is the result of exposure to risk factors over time.
These individuals then must have had one or more risk factors for a long time prior to their heart attack.
Remember.
The majority of heart attacks occur as a result of plaque in the coronary arteries that is not obstructive and, therefore, asymptomatic.2

You will not know you have heart disease by waiting for symptoms.
But why did they develop plaque so early in life?
The answer: Risk Factors.
But wouldn’t such risk factors have been obvious?
Sadly not.
We are learning that risk factors such a high LDL-C, blood pressure and average blood sugar levels, even in the high normal range, can increase cardiovascular risk.
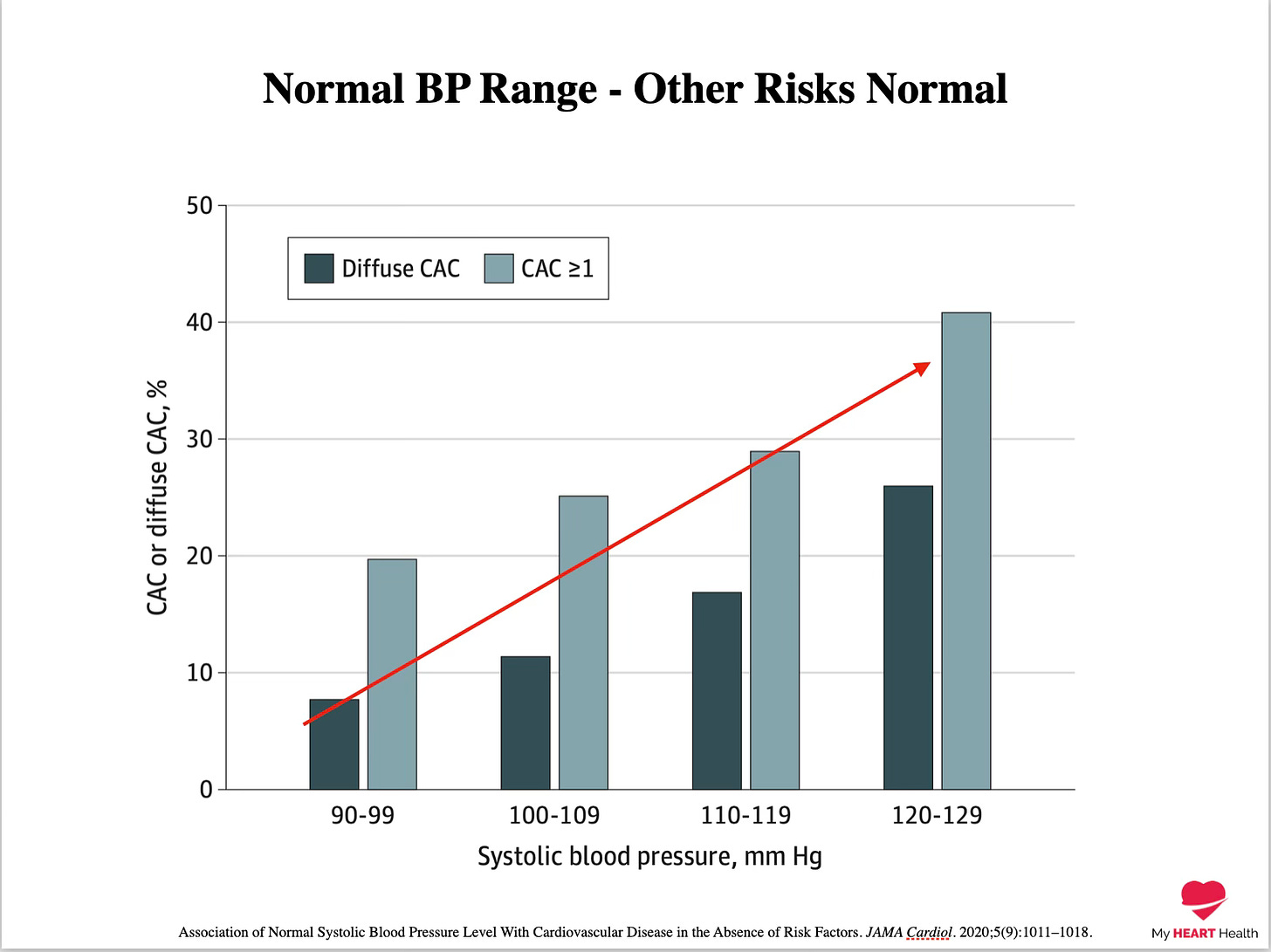
Systolic blood pressure, even above 90 mmHg, results in higher risk3.
(This does not mean we should treat blood pressure down to this target!)
The thresholds we set as ‘normal’ for risk factors such as LDL-C are likely way off too.
When evaluating cumulative exposure to ‘high normal’ levels, increasing levels of risk are identified.
The same holds true for HBA1c levels in the normal range.
For many of our traditional risk factors, normal does not mean optimal4.
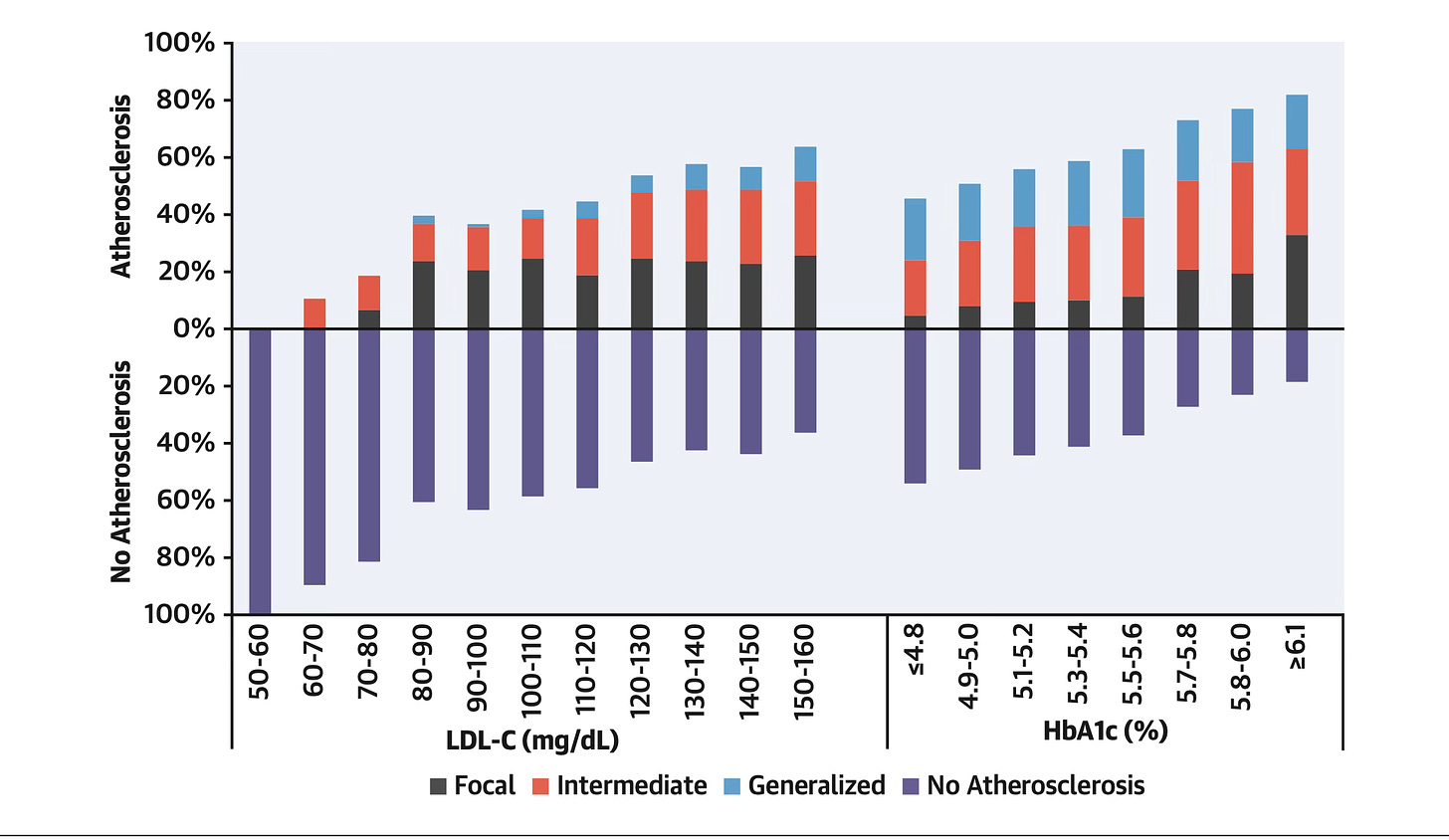
What the above graph shows is that for those with an LDL-C of 3.4 mmol/l (130 mg/dl) or below, between 20-50% will already have coronary artery disease.
For HBA1c, the trend is similar. As HBA1c increases, even in the normal range, the probability of coronary artery disease increases.
Remember, these are all in the ‘normal’ range.
And this is in people less than 50 years of age.
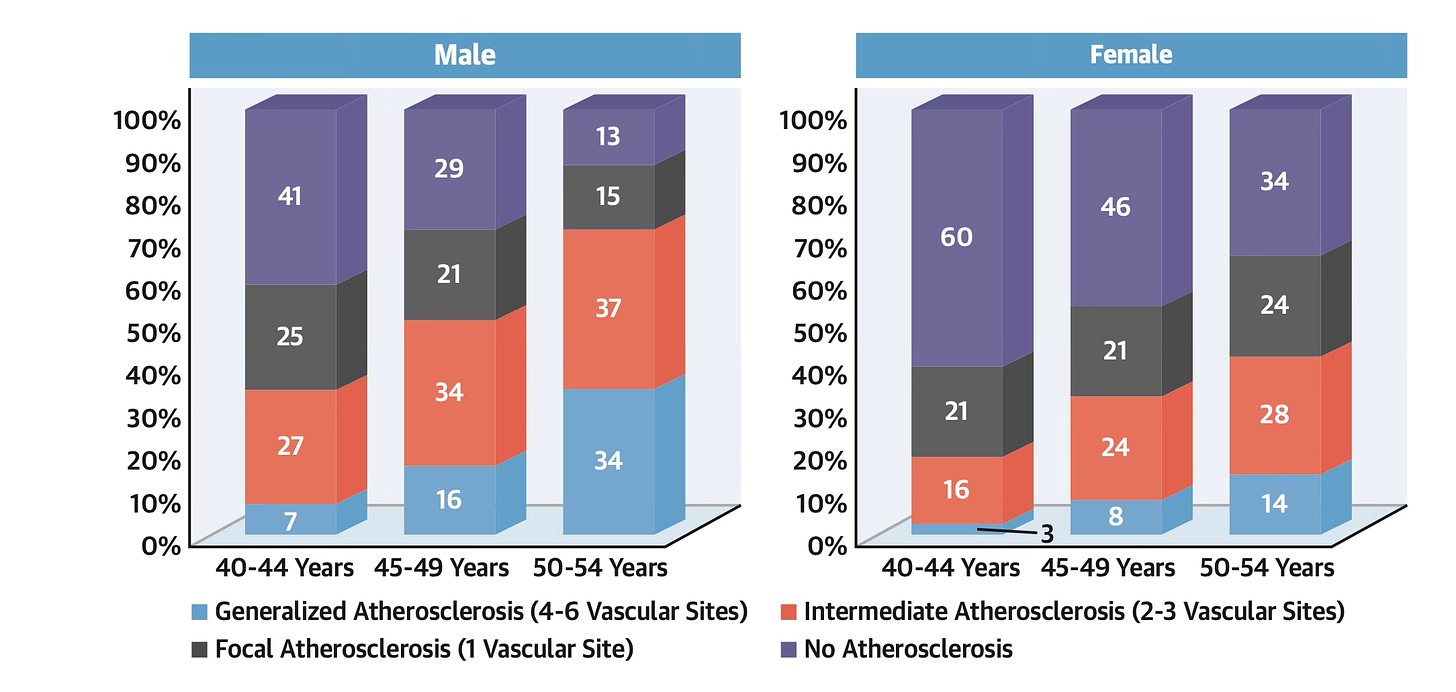
For those aged 40-44, only 40% of males and 60% of females have no evidence of plaque buildup in any vascular territory.
Risk Calculators
These risk factors, LDL-C and blood sugar levels, are often used to estimate cardiovascular risk, typically over a 10-year time frame.
Individuals are classified as either low, moderate or high risk depending on how abnormal they are, if at all.
But how well do they perform at identifying those with early plaque build-up in a vascular territory?
The answer.
Badly.
Almost 60% of those identified as ‘Low Risk’ by 10-year risk calculators already have evidence of plaque buildup in a vascular territory.
For those in the ‘Moderate Risk’ category, that figure rose to 86%5.

So far, two things should be very clear.
-
‘Normal’ levels of risk factors such as blood pressure, cholesterol or blood glucose levels are often FAR from optimal.
-
Because we are not aggressively managing these risk factors, people are developing significant amounts of plaque buildup very early in life, which seriously increases the risk of an early heart attack.
In my view, when it comes to the risk factors for heart disease, OK is not OK.
If your goal is to maximally reduce your risk of heart disease over your lifetime, then getting your cardiovascular risk profile into the optimal range is a necessity.
If ANYONE says something along the lines of:
“Your ‘Insert Risk Factor’ is a little bit high, but it’s probably ok”
they likely have no idea what they are doing.
In this instance, your risk factor is now OUTSIDE of the normal range.
Everything we have been reviewing to date has been about risk factors WITHIN the normal range.
The Missing Variable Of Time
One of the factors most often left out of cardiovascular risk discussions is the element of ‘cumulative time of exposure’.
Risk is a function of two variables.
-
How ABNORMAL is the risk factor?
-
How LONG has it been abnormal?
This is why a female who develops high LDL cholesterol much later in life is at far less risk than a female who has had high LDL cholesterol ALL of her life.
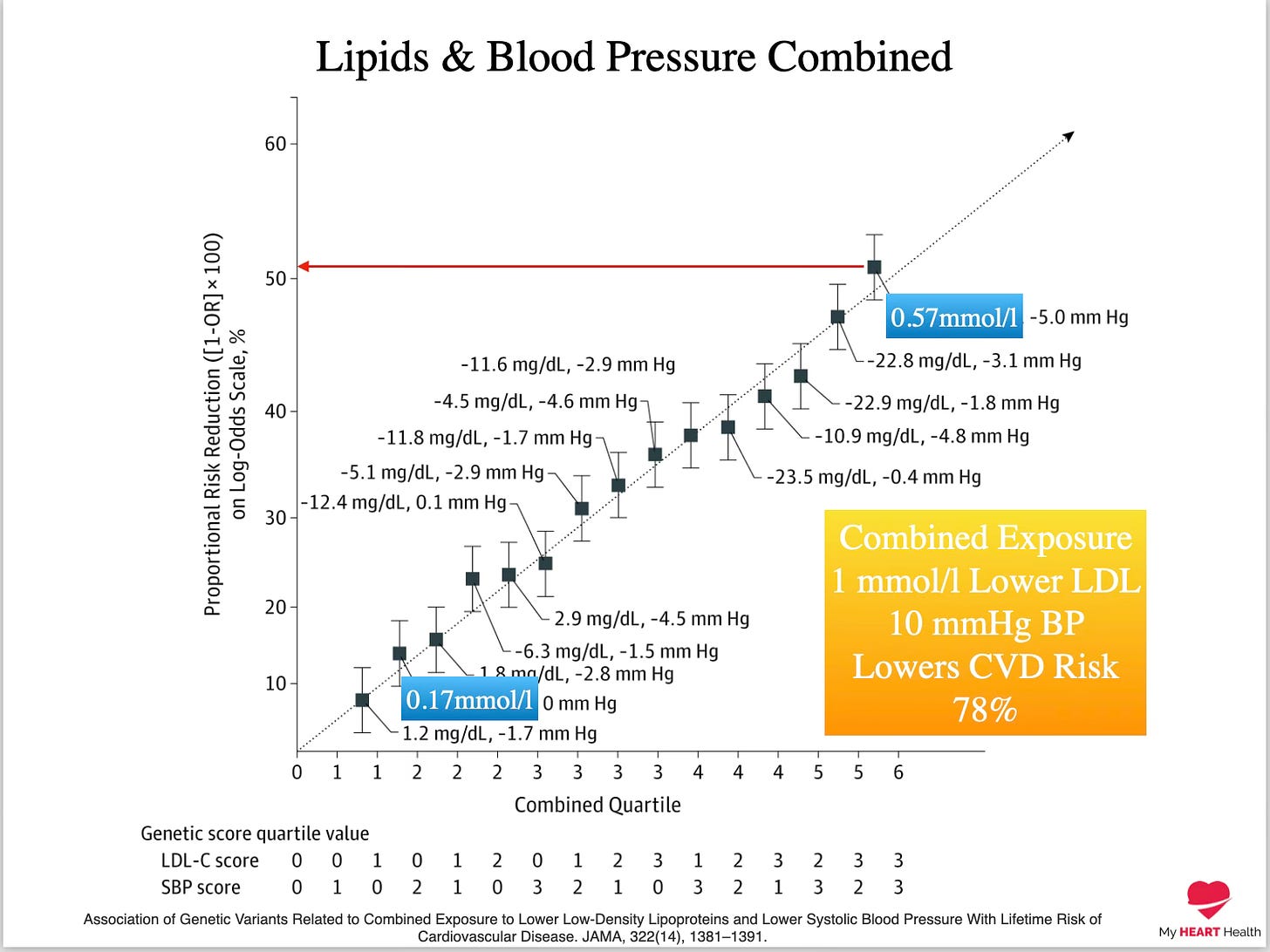
It’s the EXPOSURE TIME that is most consequential here.
This is why even modest reductions in LDL-C and blood pressure over LONG periods can result in huge reductions in cardiovascular risk.
For example, even a reduction of LDL-C by 1 mmol/l (39 mg/dl) and a 10 mmHg reduction in systolic blood pressure can reduce cardiovascular risk by 78% when considering risk over very long time horizons6.
Act Early
Most people only start to think about the risk of heart disease later in life.
Usually after age 50.
I hope it is crystal clear to you by this point that waiting until this age is WAY too late.
It’s not that you can’t make a difference.
You can.
But if you had started 30 years previously, the difference you could have made would have been much greater.
DO NOT WAIT to address the risk factors for heart disease.
Many, if not all, can be addressed with appropriate lifestyle measures.
However, some cannot and will require medications.
But regardless of HOW you address them, the earlier you address them, the better.
Risk of Premature Cardiovascular Disease vs the Number of Premature Cardiovascular Events. JAMA Cardiol. 2016;1(4):492-494.
Contemporary rationale for non-invasive imaging of adverse coronary plaque features to identify the vulnerable patient: a Position Paper from the European Society of Cardiology Working Group on Atherosclerosis and Vascular Biology and the European
Association of Cardiovascular Imaging. EuropeanHeartJournal-CardiovascularImaging(2020)21,1177–1183
Association of Normal Systolic Blood Pressure Level With Cardiovascular Disease in the Absence of Risk Factors. JAMA Cardiol. 2020;5(9):1011–1018.
Primary Prevention of Subclinical Atherosclerosis in Young Adults: JACC Review Topic of the Week. J Am Coll Cardiol. 2023 Nov, 82 (22) 2152–2162.
Prevalence, Vascular Distribution, and Multiterritorial Extent of Subclinical Atherosclerosis in a Middle-Aged Cohort: The PESA (Progression of Early Subclinical Atherosclerosis) Study. Circulation. 2015 Jun 16;131(24):2104-13.
Association of Genetic Variants Related to Combined Exposure to Lower Low-Density Lipoproteins and Lower Systolic Blood Pressure With Lifetime Risk of Cardiovascular Disease. JAMA, 322(14), 1381–1391.




